off the charts
POLICY INSIGHT
BEYOND THE NUMBERS
BEYOND THE NUMBERS
Indiana’s New Medicaid Waiver Requires Close Watch
Receive the latest news and reports from the Center
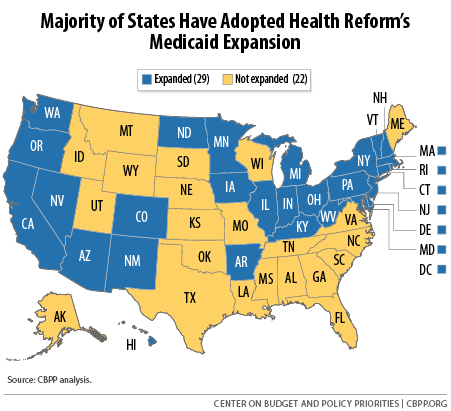
With Indiana becoming the 29th state to adopt health reform’s Medicaid expansion, we’re happy to see another state expand Medicaid (see map below) — but it remains to be seen whether Indiana will meet its coverage goals and whether enrollees will get the care they need. The Department of Health and Human Services (HHS) last week approved the Healthy Indiana Plan (HIP) 2.0 Medicaid waiver, which the state expects will cover about 350,000 uninsured Hoosiers. Last October, we wrote about several features of Indiana’s waiver proposal that could create barriers to coverage and care. Unfortunately, not much changed in the final plan. As extensive research shows, charging poor people premiums and co-payments keeps many from enrolling in coverage and getting needed medical care. Yet under its new waiver, Indiana can require poor people to pay a monthly premium to get a benefit package that includes dental and vision care. Even people with no income will have to pay $1 a month. If they don’t, the state will shift them to a plan that lacks dental and vision care and imposes $4 copayments for doctor visits and prescriptions. People at or slightly above the poverty line who don’t pay their premiums will lose coverage altogether and won’t be able to re-enroll for six months. We’ll watch closely as Indiana reports on its progress to see if the HIP 2.0 premiums and co-pays have negative impacts. HHS, too, should wait to see the results of HIP 2.0 before approving similar features in other Medicaid waivers.